Therapies that are not yet approved by the regulatory agencies like the U.S. Food and Drug Administration (FDA) in the United States are called investigational. Investigational therapies go through the drug development process, including clinical trials, before they can be prescribed to patients.
Though Ultragenyx can make its investigational therapies available to patients through early access, the primary preferred mechanism for access to investigational therapies is by participation in a clinical trial. It’s important to note that to be granted early access to an investigational medicine, the request must be initiated and driven by a physician. Read more and learn about our policy on access to investigational therapies here.
Learn more about clinical trials below.
Patient Group Engagement Across the Clinical Trial Continuum*
The Clinical Trials Transformation Initiative outlines where and how patient groups can get involved across the clinical trial continuum
Patient groups have potential to enhance the quality and efficiency of clinical trials by providing:
- Financial support for research
- Natural history data
- Input on relevance of research to patients
- Access to translational tools
- Help defining eligibility criteria
- Input on meaningful endpoints & PROs
- Advocacy for policy & funding issues✝
- Education to patient community✝
- Support to sponsors around key regulatory meetings
- Support preparing submissions for newborn screening for rare diseases
- Informing regulators on benefit-risk✝
- Public testimony at regulatory meetings✝
- Benefit-risk & patient-preference studies
- Protocol design & study feasibility input
- Study recruitment & retention strategy input
- Increased awareness about trials
- Participant feedback on trial experience
- Input on informed consent content & processes
- Peer advocates for participants✝
- Clinical trial networks✝
- Data and Safety Monitoring Board Members✝
Phase 1-3 activities and…
- Support interpreting & disseminating study results
- Collaboration on post-marketing studies & surveillance initiatives
- Support developing access strategy & preparing for value or health technology review
*Updated 2018; adapted from Parkinson’s Foundation materials | ✝Patient group activities typically undertaken independently or with partners other than sponsors | ☨Includes early planning for trials
People volunteer for clinical trials to help researchers learn about new and existing treatments. Carefully conducted clinical trials—led by medical doctors called principal investigators—are the optimal way to find new treatments.
Clinical trials are conducted at approved study sites such as hospitals, universities, doctors’ offices, and community clinics.
The following terms are commonplace in clinical trials. You may want to familiarize yourself with them to properly understand how they work.
Visit the Conditions We Study page to learn about Ultragenyx clinical trials currently enrolling
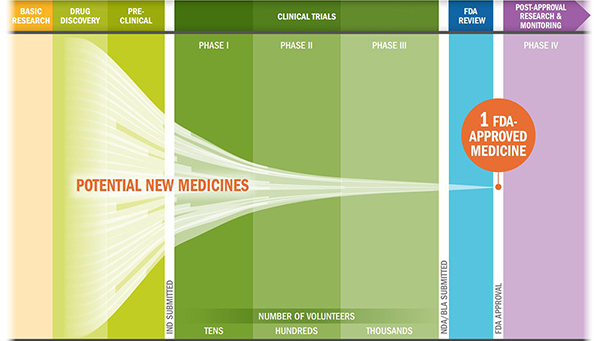
The Biopharmaceutical Research and Development Process
Protocol
Each clinical trial has a plan—known as a protocol—which must be conducted according to strict scientific and ethical principles.
Details include participation criteria—also called inclusion criteria—, test schedules, procedures, medications, and study length.
Placebo/sugar pill
Sometimes a drug undergoing investigation is compared against a placebo, also called a sugar pill.
The placebo looks like the study drug but contains no active ingredients. Using a placebo helps increase the possibility that any effects seen in the study are due only to the study drug itself.
Inclusion and exclusion criteria
Inclusion criteria are the factors that allow someone to participate in the study. Exclusion criteria are factors that prohibit someone from participating in a trial.
These criteria are part of the study protocol and help to set parameters for trial outcomes.
FDA approval process1
The development of potential treatments is divided into steps called “phases.” Generally, the trial treatment must pass through each phase successfully before it can continue to the next.
| Phase 1 | Phase 2 | Phase 3 |
|---|---|---|
| Usually healthy volunteers (although may include people with the disease) | People with the disease | People with the disease |
| Safety and how the body breaks down the study treatment | Safety and effectiveness (the ability of a trial treatment to produce a beneficial change) | Long-term safety and effectiveness compared to current standard of care or a placebo (sugar pill) |
| Phase 1 |
|---|
| Usually healthy volunteers (although may include people with the disease) |
| Safety and how the body breaks down the study treatment |
| Phase 2 |
|---|
| People with the disease |
| Safety and effectiveness (the ability of a trial treatment to produce a beneficial change) |
| Phase 3 |
|---|
| People with the disease |
| Long-term safety and effectiveness compared to current standard of care or a placebo (sugar pill) |
Once the necessary trials are complete, the trial results along with other information on the drug are submitted to and reviewed by a government agency (e.g., in the United States, the Food and Drug Administration[FDA]). If the data show the study treatment is safe and effective, it may be approved for use by prescription.2
Potential Benefits and Risks of Clinical Trial Participation
Potential benefits1
- Receiving regular, close monitoring and care from an experienced research team
- Helping others by contributing to medical research
- Gaining access to investigational treatments
- Playing an active role in your own health care
Potential risks1
- Unpleasant, serious, or even life-threatening adverse effects of the treatments being tested
- Time commitments for trial participation
- The treatment being studied may not work
Consider participating1
Taking part in a clinical trial is voluntary. That means you don’t have to join if you don’t want to and that your future health care options will not be affected if you decide that you don’t want to participate.
You can even withdraw your consent to participate in a study once you’ve joined if you change your mind.
Understanding your rights: informed consent
If you want to take part in a clinical trial, you’ll be asked to review an informed consent form (ICF).
You can still leave a trial at any time if you change your mind, even after signing the ICF.
Among other information, an ICF will tell you:
- What to expect during your time on the trial
- What tests you’ll have
- The potential risks or benefits of the trial drug
- Your rights as a study participant
You can review the ICF information with a member of the team at the trial site. They’ll answer any questions that you might have. You may also ask your doctor or a friend or family member to review the ICF.
Once your questions have been answered, you’ll be asked to sign the ICF. This shows that you understand the study’s requirements and agree to take part.
References
- Learn about clinical studies. National Institutes of Health Clinical Center. https://clinicaltrials.gov/ct2/about-studies/learn. Updated December 2015. Accessed August 17, 2016.
- Development & approval process (drugs). U.S. Food and Drug Administration. http://www.fda.gov/Drugs/DevelopmentApprovalProcess/. Updated January 2016. Accessed August 17, 2016.

